Por Klaus Langohr (Universitat Politècnica de Catalunya).
Abstract: Bone mineral density (BMD) measurements are used to determine bone health and can help to identify the risk of fracture. The most widely recognized BMD scan, which measures bone density at different parts of the body, is called dual-energy x-ray absorptiometry (DXA). The DXA measures are compared to the BMD of a healthy 30-year-old adult of the same gender and are converted into T-scores, which are used to classify BMD: T-scores above -1 are considered normal, values between -1 and -2.5 indicate low bone mass (osteopenia), and values below -2.5 indicate osteoporosis (Kanis, 1994).
The main goals of the present study are to study the evolution of BMD over time in a cohort of 875 HIV-infected persons with at least two DXA scans and to determine the risk factors for the progression of bone loss. In particular, it is of great interest to assess the risk of low bone mineral density according to the antiretroviral treatment.
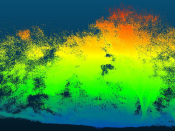
For this purpose, a bidirectional time-inhomogeneous multi-state model with three states is fitted to the data: normal BMD, osteopenia, and osteoporosis. The model considers four possible transitions (normal BMD to osteopenia, osteopenia to normal BMD, osteopenia to osteoporosis, and osteoporosis to osteopenia) that are studied as a function of age and antiretroviral treatment. Due to the nature of the panel data available, all transition times are interval-censored (van den Hout, 2016).
This multi-state model allows us to estimate the transition probabilities and the percentages of patients in every health state as a function of age and treatment. The clinical relevance of building such a model is to guide the clinical practice and to rationalize DXA scans measurements.